More than 57,000 new and expectant mums have received specialist support for mental health problems over the last year, up a third on 2022, NHS figures show.
Every part of England now has a specialist mental health team thanks to the NHS Long Term Plan, with experts offering women with moderate to severe or complex mental health needs support, including on how to develop the relationship between parent and baby.
In addition, all new mums are also offered a comprehensive mental and physical check-up from their GP, within six weeks of giving birth.
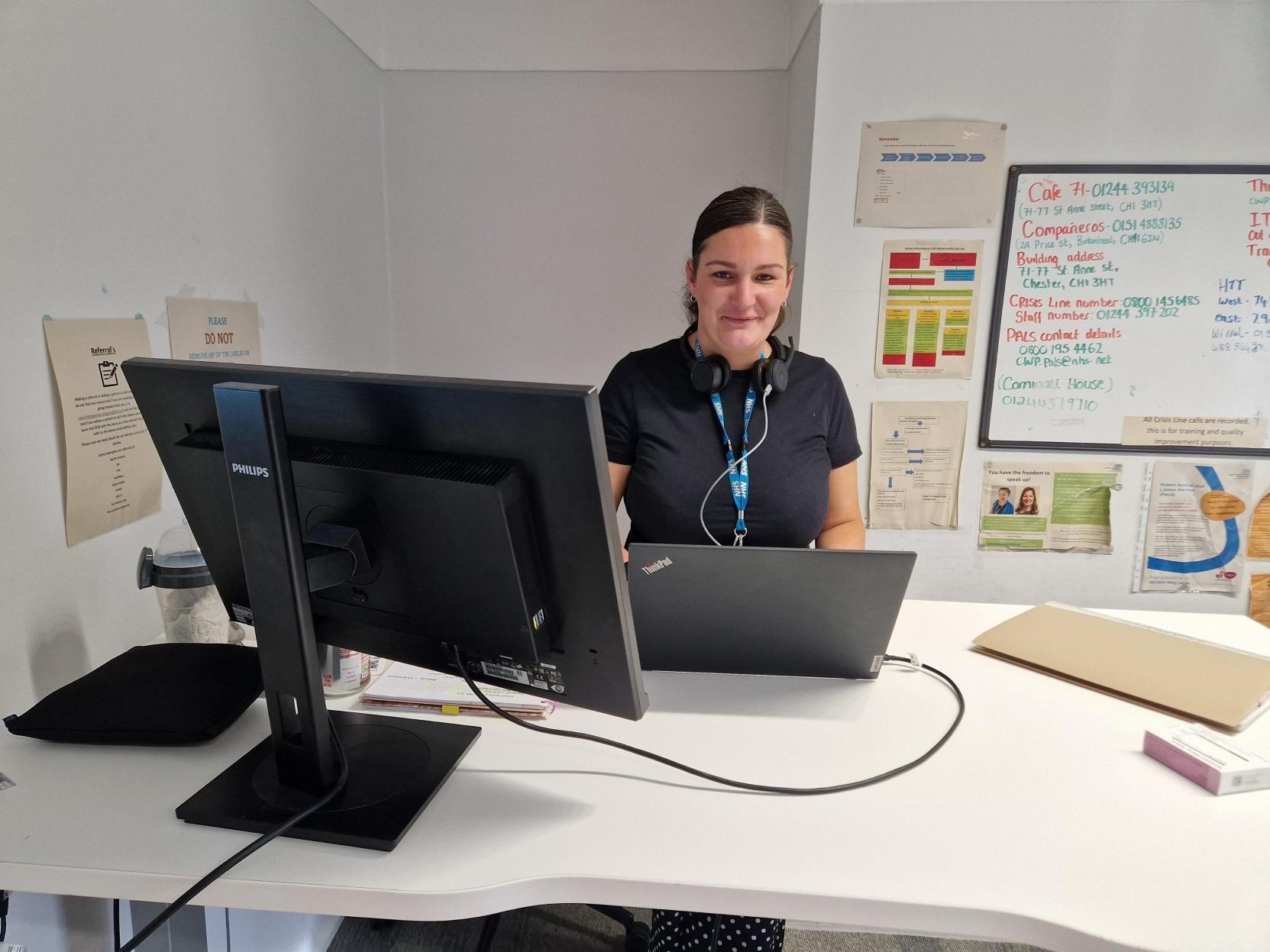
In the North West, partners from across the NHS and beyond have been working to develop and transform perinatal mental health services, with the aim of providing timely access, specialist care and support in the community. This is to ensure that the range and complexities and needs that women present with can be appropriately assessed and treated by specialist teams using specific evidence-based psychological therapies, working to deliver improved outcomes for women, babies and their families.
In the last year, over 8,000 women have been in contact with specialist perinatal mental health services across the region, with numbers increasing year on year since the introduction of the NHS Long Term Plan.
For those women who need further specialist support, their family doctor, obstetrician, midwife or health visitor can refer them to one of almost 40 Maternal Mental Health Services established across England with staff including psychologists and midwives, who are able to help with range of issues including post-traumatic stress disorder following birth trauma, perinatal loss or those with a severe fear of childbirth, with 865 women accessing these services within the last 12 months across the region.
The services also provide support and advice for women with mental health needs who want to get pregnant.
Around 600,000 women give birth in England every year and research shows perinatal mental illness affects up to one in five new and expectant mums and covers a wide range of conditions. If left untreated, mental health issues can have a long-lasting impact on the woman, child, and the wider family.
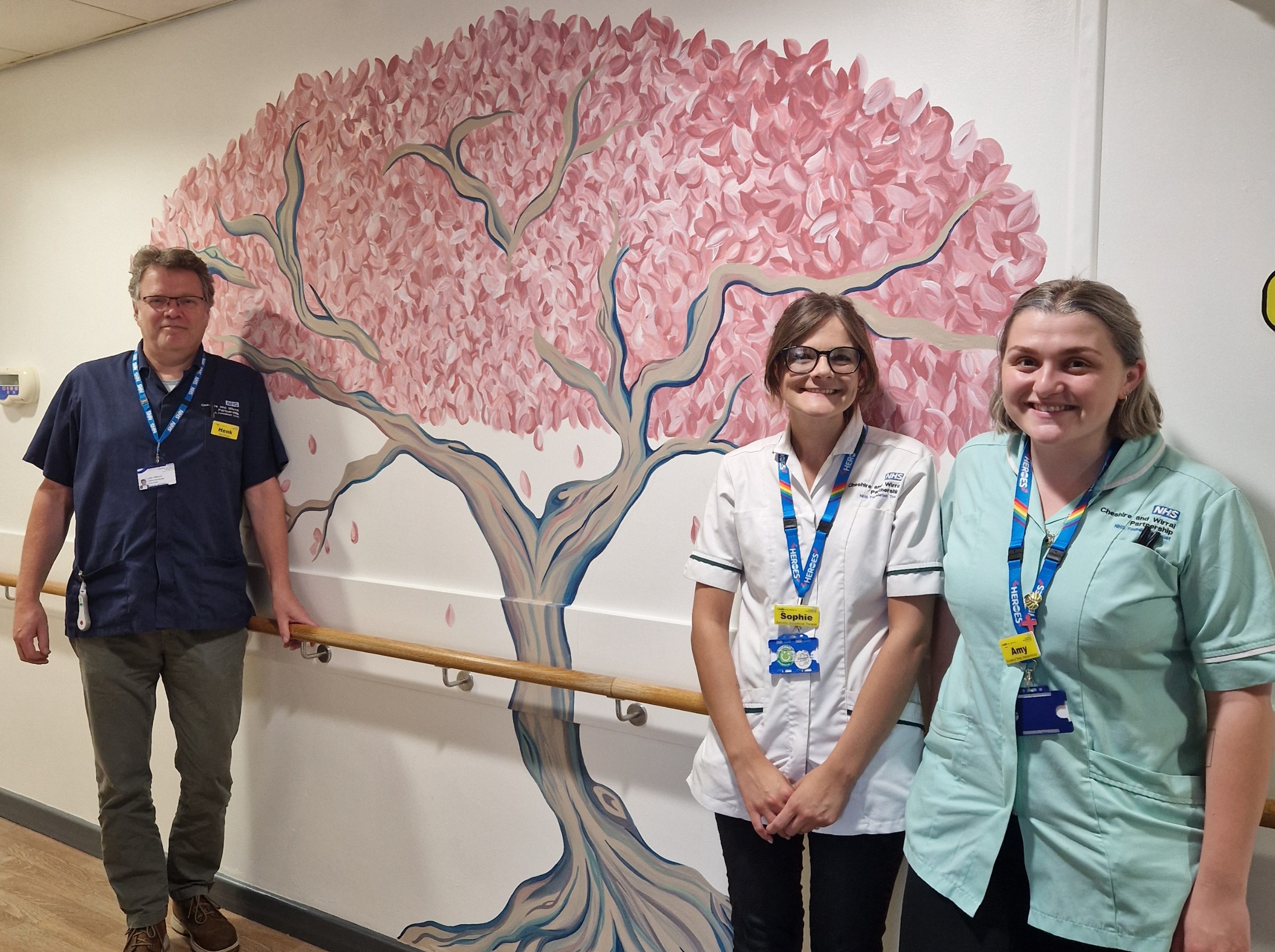
In Cheshire and Merseyside a new specialist mother and baby inpatient unit to support new and expectant parents across Cheshire, Merseyside and North Wales is due to open next year, with work starting on the building work last November.
Seren Lodge, a name chosen by mum’s who have experienced maternal mental ill-health and is a result of a partnership between Cheshire and Wirral Partnership NHS Foundation Trust (CWP), Betsi Cadwaladr University Health Board (BCHUB), Mersey Care NHS Foundation Trust, NHS England and NHS Wales will see a disused training centre transformed into a specialist, eight bedded unit for perinatal mothers, babies and their families.
Once open the unit will work alongside the existing regional Community Perinatal Mental Health service who already care for thousands of women every year.
CWP Expert by Experience, Jennifer, said: “I was first introduced to the perinatal mental health service during my second pregnancy. A few months after having my little boy I became seriously mentally unwell requiring a significant level of professional help. The care that I received from the perinatal mental health service was second to none and had it not been for their quick action and ongoing support I truly believe that I wouldn’t be here today sharing my story.
“I have always been a passionate advocate for talking about mental health. Having spent a number of years walking and talking with new mums, I recognise the importance of sharing my lived experience in bridging the gap between the person sitting where I was, not knowing where to turn, and the service provider waiting to support them.
“Stepping into the service was terrifying but once I was in, the support was like a strong, warm and secure embrace. I felt seen, heard, and most importantly, through talking to others and relating to their experience, I felt understood. Now, taking what I have been through and what I have learned on my journey, I am incredibly proud to be in a position where I can help others to feel comfortable seeking support and help shape perinatal mental health services as a member of the Cheshire and Merseyside Mother Baby Unit Lead Provider Collaborative Forum.
“If you’re reading this and you’re wondering if the service could help, please reach out. You are not alone. You can do this. We are here for you.”
Claire Mathews, Regional chief midwife for NHS England – North West, said: “To help ensure women are well supported during their transition to becoming a parent, they should be offered personalised care during and after pregnancy that takes account of not only their physical health and choices, but importantly their mental health too. This is facilitated in the North West by having a specialist community perinatal mental health team in all three of our local health systems and for which access is increasing.
“In the most recent CQC maternity survey for 2023 more women than ever before were positive about mental health support – with almost all saying a midwife or health visitor asked them about their mental health during postnatal care at home.”
The NHS published further guidance for GPs on these check-ups in December.
The guidance, written together with the RCGP, asks family doctors to provide personalised postnatal care for their physical and mental health, covering topics such as mental health, physical recovery, pelvic health, breastfeeding and support with family planning.
The routine check is an opportunity for GPs to ask women about their mental health and wellbeing, as well as physical recovery, post-birth. It means any woman needing extra mental health support can be referred to primary care mental health support including Talking Therapies or to a specialist perinatal mental health team, if appropriate.